Trigeminal Neuralgia
- Excruciating, stabbing pain of the face or jaw, which can feel like an electrical shock.
- Numbness, tingling, or a burning sensation on one side of the face.
- Facial pain accompanied by a muscle spasm, or “tic.”
- Face or jaw pain that is triggered by simple, everyday acts such as shaving, applying make-up, brushing teeth, chewing, talking, and touching the face.
- Pain that is isolated to one side of the face, including the jaw, cheek, gums, mouth, and sometimes the forehead and eye.
- Pain that is concentrated in one small area — or alternatively, spread over a large area of the face.
- Attacks of pain that can last for a few seconds up to several minutes.
- Repeated episodes that can last for days, weeks, months, or longer.
- Episodes that increase in intensity, duration, and frequency.
- Pain related to trigeminal neuralgia is sudden, shock-like and brief.
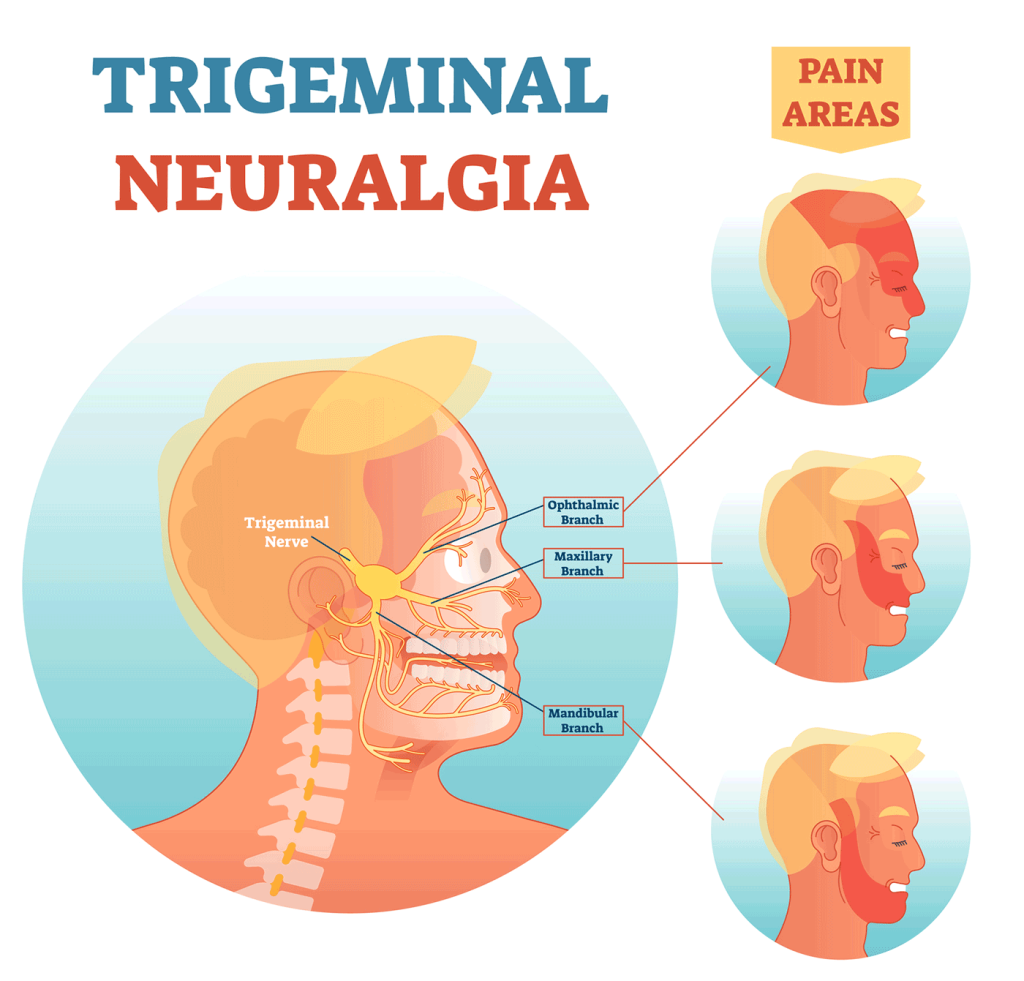
- The parts of your face that are affected by pain will tell your doctor if the trigeminal nerve is involved.
- Trigeminal neuralgia-related pain usually is brought on by eating, talking, light touch of your face or even encountering a cool breeze.
- A neurological examination.Touching and examining parts of your face can help your doctor determine exactly where the pain is occurring and — if you appear to have trigeminal neuralgia — which branches of the trigeminal nerve may be affected. Reflex tests also can help your doctor determine if your symptoms are caused by a compressed nerve or another condition.
- Magnetic resonance imaging (MRI).Your doctor may order an MRI scan of your head to determine if multiple sclerosis or a tumor is causing trigeminal neuralgia. In some cases, your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow.
Microvascular Decompression (MVD)
Microvascular decompression is an open surgical procedure that involves moving or removing the blood vessels that are creating pressure on the trigeminal nerve. The neurosurgeon will make an incision behind the ear on the side that is causing pain, exposing the trigeminal nerve, then removes or relocates any blood vessels that are compressing the nerve or inserts a small pad to prevent contact with the nerve. If no blood vessels are compressing the nerve, the surgeon will conduct a rhizotomy to sever the nerve itself.
Stereotactic Radiofrequency Lesion (RFL)
Stereotactic radiofrequency lesion (RFL) is a less invasive procedure than microvascular decompression. A radiologist and neurosurgeon collaborate to pinpoint the exact location of the nerve, then use high heat to destroy only the pain portions of the trigeminal nerve, leaving other sensation intact. Pain relief is usually immediate (or within 48 hours); in some patients the procedure may be repeated several times until adequate pain relief is achieved.
Stereotactic Radiosurgery
Stereotactic radiosurgery is not surgery in the conventional sense, but rather a non-invasive specialty that does not involve any cutting at all. It consists of directing beams of highly focused radiation at a specific target in this case, the trigeminal nerve. The radiation beam damages the trigeminal nerve, but does not destroy it completely. Pain relief occurs gradually, over the course of a few weeks. The results are usually long-lasting, and the treatment can be repeated in the case of recurrence. The GammaKnife is one type of stereotactic radiosurgery treatment it’s a completely painless, highly effective treatment that can be performed on an outpatient basis.
